- Anúncios -
O que significa skill?
Você já se perguntou o que significa skill? É uma palavra pequena, mas com um significado grande. Skill é a habilidade que temos para realizar diferentes tarefas ou alcançar objetivos específicos. Ela envolve conhecimento, prática e aperfeiçoamento contínuo. Nossas skills nos definem e nos destacam em nosso caminho para o sucesso. Descubra quais são as suas e potencialize suas conquistas!
O que significa float?
Float é um termo inglês que muitas vezes confunde as pessoas. Mas não se preocupe, estamos aqui para desvendar esse mistério. Float, no contexto da programação, se refere a um tipo de dado que representa números de ponto flutuante, ou seja, números com vírgula. Agora que você sabe o significado, pode mergulhar de cabeça no mundo da programação!
O que significa roughly?
O que significa 'roughly'? Essa palavra intriga muitos falantes de português, mas seu significado é, digamos, aproximado. Como jogar dardos em uma parede e esperar que eles acertem o alvo. Então, quando você ouvir 'roughly', não se preocupe em ser preciso. Apenas dê o seu melhor palpite e siga em frente!
Medicina
O quê significar ser nórdico?
Ser nórdico é ser enraizado nas paisagens gélidas, nas histórias de gigantes…

Create an Amazing Newspaper
Siga-nos
O que significa assunto na matemática?
Matemática, a pedra angular do conhecimento numérico, muitas vezes nos desafia com…
O que significa atrito na matemática?
Uma sensação de hesitação e resistência surge quando dois corpos se encontram,…
O que significa arco na matemática?
Na matemática, o arco é um elemento fundamental que nos leva a…
O que significa logaritmo na matemática?
O logaritmo, um conceito matemático tão enigmático quanto fascinante, desvenda os segredos…
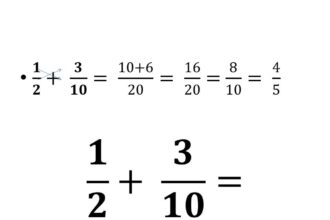
O que significa denominador?
Você já se perguntou o que significa denominador? Uma palavra tão peculiar…
O que significa áreas de figuras geométricas?
Desde os tempos antigos, figuras geométricas têm sido um fascínio para os…
O que significa expressão numérica?
A expressão numérica, um enigma matemático envolto em símbolos, números e operações.…
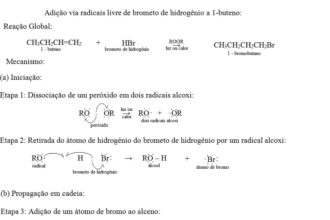
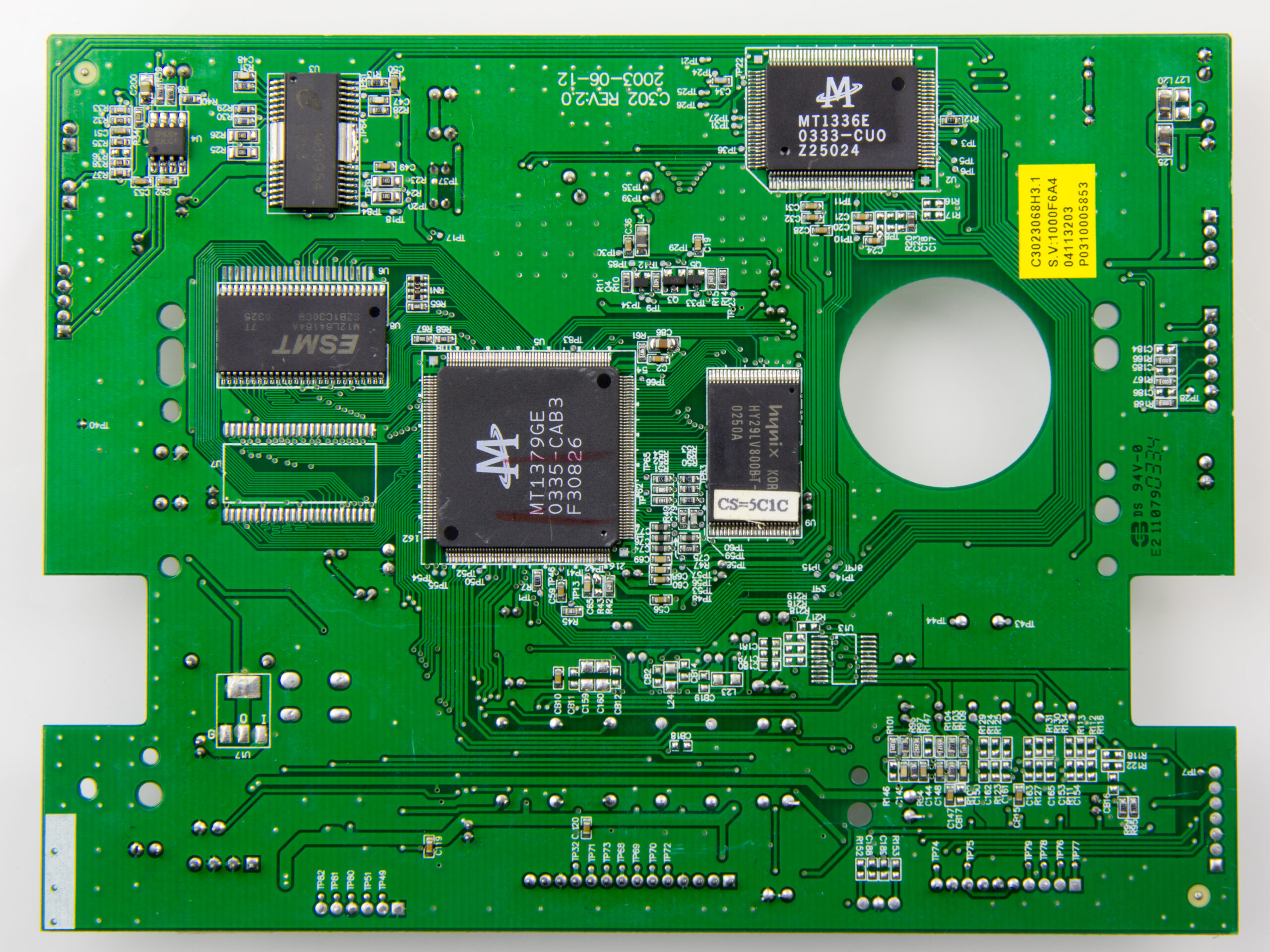
O que significa algoritmo?
Você já ouviu falar em algoritmo, mas sabe o que isso realmente…

Create an Amazing Newspaper
Conteúdo patrocinado
O que significa capitalismo?
O que significa capitalismo? É um conceito que se desdobra em um verdadeiro oceano de interpretações e debates. Desde sua origem na Revolução Industrial até os dias atuais, o capitalismo abrange os pilares da propriedade privada, da livre iniciativa e do mercado competitivo. Mas, será que esse sistema econômico tem se mostrado eficiente e sustentável para todos? Exploraremos essas questões e muito mais neste artigo, mergulhando nas profundezas desse complexo sistema que molda nossa sociedade contemporânea.
O que significa IDK?
Você já se deparou com a sigla "IDK" e ficou se perguntando o que significa? Bem, IDK é a abreviação para a expressão em inglês "I don't know", que traduzida…
Top Autores
Stay Up to Date
Subscribe to our newsletter to get our newest articles instantly!