- Anúncios -
O que significa station?
Estação, uma palavra simples que carrega consigo um mundo de significados. Das estações do ano às estações de trem, cada contexto traz consigo uma história única. Mas será que a palavra "station" tem o mesmo significado em todos os lugares? Explore conosco o significado de station em diferentes contextos e descubra sua vastidão linguística. Pronto para embarcar nessa jornada?
O que significa hunting?
Caçar, uma prática ancestral, carrega consigo significados que transcendem a mera busca por alimento. É a conexão com a natureza, o desafio pessoal e a valorização da preservação. Descubra nesse artigo o verdadeiro significado de caçar e como essa atividade influencia nossa relação com o ambiente ao nosso redor.
O que significa important?
O que significa important? Essa é uma pergunta que pode nos levar a uma busca profunda de reflexão. Ser importante não se resume apenas a ter poder ou influência, mas sim a fazer a diferença na vida de alguém. É sobre ser valioso e ter um propósito. Descubra o seu significado de importante e perceba que ele está além das…
Medicina
O que significa ter mal de Parkinson?
Mal de Parkinson é uma encruzilhada do destino. Um intruso invisível que…

Create an Amazing Newspaper
Siga-nos
O que significa dividendo?
Você já se perguntou o que significa dividendo? Essa é uma palavrinha…
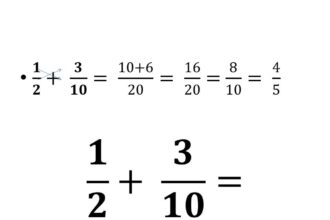
O que significa multiplicação?
A multiplicação é como uma poção mágica matemática que transforma um número…
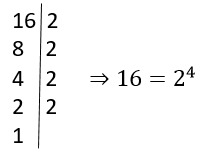
O que significa algoritmo?
Você já ouviu falar em algoritmo, mas sabe o que isso realmente…
O que significa logaritmação?
Você já se deparou com o termo "logaritmação" e ficou se perguntando…
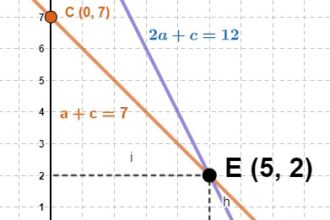
O que significa função afim na matemática?
A função afim na matemática é como uma dança matemática encantadora, na…
O que significa logaritmo na matemática?
O logaritmo, um conceito matemático tão enigmático quanto fascinante, desvenda os segredos…
O que significa antilogaritmo na matemática?
Antilogaritmo, uma palavra intrigante no mundo da matemática. Mas o que será…
O que significa denominador?
Você já se perguntou o que significa denominador? Uma palavra tão peculiar…

Create an Amazing Newspaper
Conteúdo patrocinado
O que significa capitalismo?
O que significa capitalismo? É um conceito que se desdobra em um verdadeiro oceano de interpretações e debates. Desde sua origem na Revolução Industrial até os dias atuais, o capitalismo abrange os pilares da propriedade privada, da livre iniciativa e do mercado competitivo. Mas, será que esse sistema econômico tem se mostrado eficiente e sustentável para todos? Exploraremos essas questões e muito mais neste artigo, mergulhando nas profundezas desse complexo sistema que molda nossa sociedade contemporânea.
O que significa ENEM?
Você já se perguntou o que significa ENEM? Essa sigla tão conhecida pelos estudantes brasileiros tem um significado importante: Exame Nacional do Ensino Médio. Descubra nessa matéria tudo sobre o…
Top Autores
Stay Up to Date
Subscribe to our newsletter to get our newest articles instantly!