- Anúncios -
O que significa gray?
O cinza, essa cor que parece flertar entre o preto e o branco, carrega consigo um mistério fascinante. O que significa gray vai muito além da simples definição de uma cor; é um convite para explorar a complexidade e nuances do mundo ao nosso redor. Seja na moda, na decoração ou nas emoções, o cinza é um símbolo de equilíbrio,…
O que significa saving?
Saving é o ato de reservar uma parte do seu dinheiro para o futuro. É uma prática financeira fundamental para criar segurança e estabilidade. Mesmo pequenos valores guardados podem fazer grande diferença no longo prazo.
O que significa due?
Você já se perguntou o que significa "Due"? Esse termo italiano é comumente usado para indicar um prazo ou vencimento. Descubra mais sobre suas diversas interpretações e aplicações em nosso artigo.
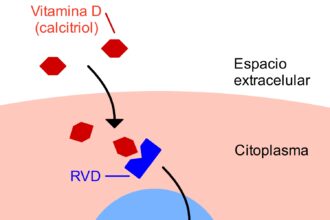
Medicina
O que significa ter colesterol alto?
Ter colesterol alto significa ter níveis elevados de lipídios no sangue, o…

Create an Amazing Newspaper
Siga-nos
O que significa equação?
O que significa equação? Quando mergulhamos no universo da matemática, nos deparamos…
O que significa antilogaritmo na matemática?
Antilogaritmo, uma palavra intrigante no mundo da matemática. Mas o que será…
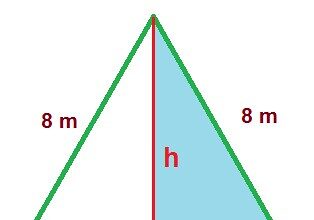
O que significa equilátero?
No mundo da geometria, a palavra "equilátero" evoca harmonia, perfeição e equidade.…
O que significa arco na matemática?
Na matemática, o arco é um elemento fundamental que nos leva a…
O que significa determinante na matemática?
O que significa determinante na matemática? O determinante é uma medida especial…
O que significa equações exponenciais?
Você já se perguntou o que significam equações exponenciais? Essas equações misteriosas,…
O que significa aproximação na matemática?
A aproximação na matemática é uma poderosa ferramenta que nos permite obter…
O que significa assunto na matemática?
Matemática, a pedra angular do conhecimento numérico, muitas vezes nos desafia com…

Create an Amazing Newspaper
Conteúdo patrocinado
O que significa capitalismo?
O que significa capitalismo? É um conceito que se desdobra em um verdadeiro oceano de interpretações e debates. Desde sua origem na Revolução Industrial até os dias atuais, o capitalismo abrange os pilares da propriedade privada, da livre iniciativa e do mercado competitivo. Mas, será que esse sistema econômico tem se mostrado eficiente e sustentável para todos? Exploraremos essas questões e muito mais neste artigo, mergulhando nas profundezas desse complexo sistema que molda nossa sociedade contemporânea.
O que significa MDF-e?
O MDF-e, ou Manifesto Eletrônico de Documentos Fiscais, é um elo tecnológico essencial para a logística das operações de transporte de carga no Brasil. Ao unificar e eletronicamente registrar informações…
Top Autores
Stay Up to Date
Subscribe to our newsletter to get our newest articles instantly!